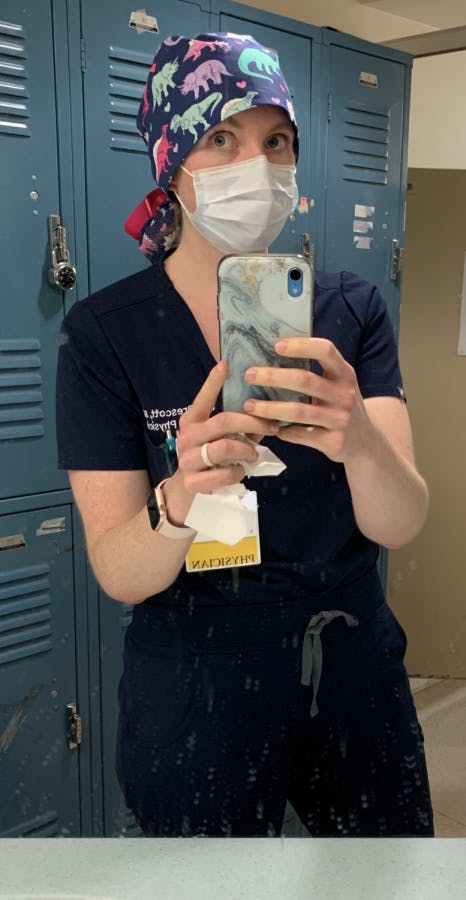
Amy Prescott '12
Location: Arlington, Virgina
Submitted April 3, 2020
As a resident physician in Emergency Medicine, I didn't expect to be coming of age in my medical career during a global pandemic. When coronavirus was still a whisper, my day-to-day was much the same as it had been. I worked shifts in the Emergency Department, taking care of patients with strokes and chest pain, before grabbing tacos with my co-residents and talking about our latest big saves and plans for upcoming vacations. Slowly, once the virus spread to the U.S. and stories came out about its devastation in Italy, things started to change. Disaster and contingency planning emails arrive daily, now-virtual weekly lectures have a dedicated Covid-19 updates hour, and, like the rest of my colleagues, I've been trying to learn as much about this disease as possible.
I work in Washington D.C., and it feels like the whole city is still waiting for the other foot to drop. It is terrifying to talk with my physician friends in New York, where the healthcare system has been overwhelmed by the sheer number of critically ill patients, and where I fear we're heading over the next few weeks. Volumes in our ED initially dropped dramatically, but the patients have been, on average, much "sicker"--they have more co-morbidities and present a diagnostic challenge, as Covid-19 can look like a heart failure exacerbation, pulmonary embolism, or so many other life-threatening conditions. It's particularly frustrating as a resident, as I'm at a point in my training where I have the knowledge and skills to take care of critically ill patients, but this disease is something brand new. I spoke with one of my attendings about how I feel like I've become less efficient and less confident over the past few weeks, as guidelines on everything from PPE to testing to management seem to change daily. He affirmed that this is how almost everyone, even doctors with 20+ years of experience, is feeling.
A few days ago, I started a rotation in the ICU, where many of the patients are admitted for Covid-19. It's frightening how quickly things can take a turn for the worse and how many of the usual therapies don't work as expected. By far the most vicious aspect of this disease is the isolation. To prevent further spread, visitors aren't allowed, and that means delivering the worst news of someone's life — that their husband, their mother, their sister has died — over the phone. I fear that I'll be having that conversation dozens of times in the coming weeks.
What has been your greatest worry or day-to-day concern as coronavirus has spread?
My two biggest worries are inadvertently infecting a family member or losing one of my work colleagues, who have been my battle buddies for the past two years of residency.
What has made you happy over the past few weeks?
I went for a bike ride on my last day off and it made me peacefully nostalgic for rides with my Midd friends, where we'd go to Vergennes Laundry and get cookies for the ride back to campus. I've been spending more time talking with my friends, and my husband and I are puppy-proofing our house for a new arrival next month.
Amy Prescott '12 in Arlington, Virginia

The bare minimum PPE I'm wearing these days, for non-Covid-19 patients.
Comments